The knee joint is the most common location of a degenerative-dystrophic disease, which is characterized by gradual destruction of cartilage with consequent changes in the articular surfaces, which is accompanied by pain and reduced mobility.

The disease is more likely to affect women over 40, especially those with overweight and varicose veins of the lower extremities.
The knee joint consists of three compartments:
- through leg?
- lateral tibia?
- supra-patellar-femoral.
These compartments can be affected by deforming osteoarthritis (DOA) both individually and in combination. 75% of all cases of knee fractures are the destruction of the inner tibial compartment (during the movements, it faces a load that exceeds the body weight by 2-3 times).
In young patients, only one joint is damaged more often - the right or left (right or left knee joint).
Causes of DOA of the knee joint
Several factors may be involved in the development of degenerative cartilage changes at the same time:
- mechanical overload of the knee joint (certain specialties, sports) with small cartilage injury.
- consequences of injuries, surgeries (meniscectomy).
- inflammatory diseases of the knee (arthritis).
- anatomical inconsistencies of the articular surfaces (dysplasia).
- violation of statics (flatfoot, curvature of the spine).
- chronic hemorrhage (accumulation of blood in the joint cavity).
- metabolic pathology (gout, hemochromatosis, chondro calcification).
- overweight;
- violations of the blood supply to the bones.
- osteodystrophy (Paget's disease);
- neurological diseases, loss of sensation in the extremities.
- endocrine disorders (acromegaly, diabetes, amenorrhea, hyperparathyroidism).
- genetic predisposition (generalized forms of osteoarthritis).
- violation of the synthesis of collagen type II.
But in 40% of cases, it is impossible to determine the root cause of the disease (primary arthropathy).
Pathogenesis of knee joints
primary stage
In the early stages of the disease, the processes of cartilage metabolism are disrupted. The composition and quality of the main building block of cartilage tissue, proteoglycans, which are responsible for the stability of the collagen network structure, are reduced.
As a result, chondroitin sulfate, keratin, hyaluronic acid are flushed out of the grid and structurally defective proteoglycans can no longer hold water. It is absorbed into collagen, the swollen fibers of which lead to a reduction in cartilage resistance to stress.
In the joint cavity, pro-inflammatory substances accumulate, under the influence of which the cartilage is destroyed even faster. Joint capsule fibrosis develops. The change in the composition of the synovial fluid makes it difficult to supply nutrients to the cartilage and reduces the slippage of the synovial surfaces during movement.
The evolution of pathology
In the future, the cartilage gradually becomes thinner, becomes rougher, cracks are formed throughout its thickness. Bone epiphyses show an increased load, which causes the development of osteosclerosis and compensatory proliferation of bone tissue (osteophytes).
This reaction of the body aims to increase the area of the joint surfaces and to redistribute the load. However, the presence of osteophytes increases the discomfort, the deformity and further restricts the mobility of the limb.
Small fractures form in the thickness of the bone, which injure the blood vessels and lead to intraosseous hypertension. In the last stage of osteoarthritis, the joint surfaces are completely exposed, deformed, the movements of the limbs are severely limited.
Knee joint symptoms
Arthropathy of the knee joint is characterized by chronic, slow progressive course (months, years). The clinic is growing gradually, without severe exacerbations. The patient can not remember exactly when the first symptoms appeared.
Clinical manifestations of knee joint:
- pain. At first, diffuse, short (with prolonged standing, climbing stairs) and as osteoarthritis progresses, the pain becomes local (front and inner surface of the knee), their intensity increases.
- local sensitivity to touch. Mainly inside the knee along the edge of the joint space.
- crunching. In stage I it may not be heard, in stage II-III it accompanies all the movements.
- tumor growth, knee deformity. As a result of the weakening of the lateral ligaments, a person develops an O-shaped configuration of the limbs (it is clearly visible even in the photo).
- restriction of mobility. At first, there are difficulties with bending the knee, later - with extension.
Causes of pain in the DOA:
- mechanical abrasion of damaged joint surfaces.
- increased intraosseous pressure, venous congestion.
- arthritis accession;
- changes in the periarticular tissues (dilation of the capsule, ligaments, tendons).
- thickening of the periosteum.
- dystrophy phenomena in adjacent muscles.
- fibromyalgia?
- compression of the nerve endings.
In contrast to coxarthrosis, the DOA of the knee may show spontaneous remission of symptoms.
Clinical manifestations of gonarthrosis depending on the stage:
| Characteristics | tent | Stage II | Stage III |
|---|---|---|---|
| Pain | Short, most often occurs when the knee is stretched (prolonged standing, walking on stairs) | Moderately, disappears after a night's rest | Intense, annoying even at night |
| Restriction of mobility | Not visible | There is restriction of expansion, mild lameness | Persistent flexion-extension contractions, lameness |
| crunching | Not | Sensible to the touch when moving | remote stinging |
| Deformation | It is missing | Slight deviation of the limb axis forward, muscle loss | Valve or valve deformation. The joint is unstable, atrophy of the thigh muscles |
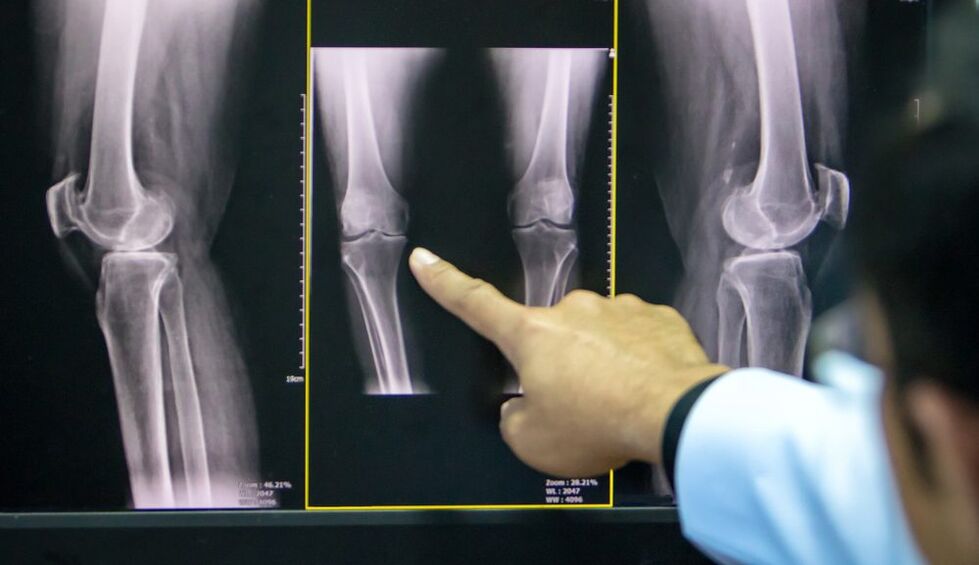
| X-ray image | Slight narrowing of the joint space, initial signs of hypochondriac osteosclerosis | The joint space narrows by 50% or more, osteophytes appear | Almost complete absence of joint space, significant deformity and hardening of joint surfaces, subchondral bone necrosis areas, osteoporosis |
A common complication of knee joint arthritis is secondary reactive arthritis, which is characterized by the following symptoms:
- increasing pain;
- οίηση;
- collection in the articular cavity.
- increase in skin temperature.
Less common and more dangerous complications include: joint blockage, osteonecrosis of the femoral condyle, patellofemoral dislocation, spontaneous hemorrhage.
DOA diagnosis of the knee joint
The diagnosis of knee joint is based on the patient's characteristic complaints, the changes detected during the examination and the results of additional examinations.
To confirm osteoarthritis, it is prescribed:
- X-ray of the knee joint in two views (anteroposterior and lateral): the most accessible way to confirm the diagnosis at an advanced stage of the pathology.
- Ultrasound: determination of the presence of collection in the joint, measurement of cartilage thickness.
- analysis of synovial fluid;
- diagnostic arthroscopy (visual evaluation of cartilage) with biopsy.
- computed tomography and magnetic resonance imaging (CT, MRI): the best method for diagnosing DOA in the early stages.
If the doctor has doubts about the diagnosis, he can prescribe:
- scintigraphy: scanning the joint after insertion of a radioactive isotope.
- thermography: study of the intensity of infrared radiation (its power is directly proportional to the power of inflammation).
Treatment of the knee joint of the knee joint
The osteoarthritis treatment regimen combines several approaches: non-pharmacological methods, pharmacotherapy and surgical correction. The proportion of each method is determined separately for each patient.
Non-drug treatment
In the latest ESCEO (European Society for Clinical Aspects of Osteoporosis and Osteoarthritis) guidelines on how to treat osteoarthritis of the knee, experts place great emphasis on educating patients and modifying their lifestyle.

The patient needs:
- Explain the essence of the disease, which is set for long-term treatment.
- teach how to use assistive devices (sticks, orthoses).
- prescribe a diet (for patients with a body mass index greater than 30).
- give a set of exercises to strengthen the thigh muscles and unload the knee joint.
- Explain the importance of increased physical activity.
In the early stages of knee arthropathy, physiotherapy methods give good results:
- massage;
- magnetotherapy?
- UHF treatment?
- electrophoresis?
- hydrogen sulfide baths?
- paraffin applications;
- acupuncture.
Pharmacotherapy of the knee joint
The use of drugs in the DOA aims to relieve pain, reduce inflammation and slow down the rate of cartilage destruction.
Symptomatic treatment:
- analgesics?
- non-steroidal anti-inflammatory drugs (NSAIDs) of the COX-2 inhibitor group in the form of tablets or suppositories.
- non-narcotic analgesics (with persistent pain syndrome).
Structure-modifying drugs (chondroprotectants):
- Chondroitin sulfate?
- Glucosamine sulfate.
These drugs can be taken in the form of capsules in courses several times a year, by injection intramuscularly or directly into the joint cavity.
Topical treatment includes proximal and intra-articular injections of glucocorticosteroids, hyaluronic acid preparations.
In stages I-II of the DOA, the use of anti-inflammatory ointments, gels and creams based on NSAIDs plays an important role in the complex treatment. They help reduce the patient's need to take NSAIDs orally, thus reducing the risk of damage to the digestive system.
Folk remedies
The use of tinctures, decoctions, extracts, topical applications of medicinal plants should be considered as adjunctive methods for the treatment of DOA, folk remedies can not replace the treatment prescribed by the doctor.
Plants used in osteoarthritis: dandelion, ginger, Jerusalem artichoke, burdock, garlic, sea buckthorn.
Surgery
Surgery may be required at all stages of the knee joint with insufficient effect of medical measures. The most common are endoscopic surgeries, in the most severe cases it is advisable to replace the endoprosthesis.

Types of endoscopic interventions:
- Joint review and repair: extraction of inflammatory contents from the articular cavity, cartilage fragments.
- Plasma or laser removal: removal of mechanical obstructions in the joint cavity.
- chondroplasty.
Corrective periarticular osteotomy is indicated for patients with initial manifestations of axial deformity (not more than 15-20%).
The purpose of the operation is to restore the normal configuration of the joint, the uniform distribution of the load on the joint surface and the removal of the damaged areas. This procedure allows you to delay arthroplasty.
Indications for replacing the affected area (or the entire joint) with artificial:
- DOA II-III grade;
- severe axial deformity of the limb.
- aseptic necrosis of the subchondral bone layer.
- persistent pain syndrome.
Contraindications to knee arthroplasty:
- total joint damage.
- unstable coupling device.
- DOA as a consequence of inflammatory arthritis.
- persistent flexion contraction, severe muscle weakness.
In this case, the patient undergoes arthrodesis - a comparison of the knee joint in a normal position with the removal of the articular surfaces. This relieves pain but shortens the leg, causing minor damage to the unilateral knee, hip and spine.
Prevention
Prevention of premature cartilage degeneration should begin in childhood.
Precautionary measures:
- scoliosis prevention;
- flatfoot correction (shoes with arch supports).
- regular physical education (limit heavy sports).
- exclusion of fixed postures at work.



























